Head and neck radiation is frequently used as primary treatment of head and neck cancers. Head and neck cancers occur in the naso-pharynx, oropharynx, hypopharynx, larynx, oral cavity and nodal basins. Primary treatment of head and neck cancers with radiation is intended as organ and function preserving treatment of early stage or locally advanced and inoperable cancers. The primary goal is to preserve speech and swallowing.
Radiation treatmetn of the head and neck is a highly morbid treatment, especially when used with concurrent chemotherapy. Radiation sequalae include xerostomia, progressive edema and fibrosis which can lead to long term problems with speech and swallowing functions. In severe cases, these sequalae can and do compromise nutrition, airway protection and quality of life.
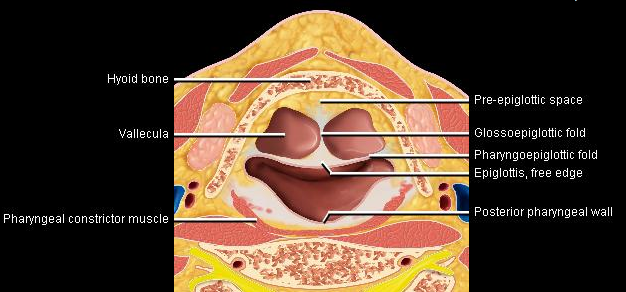
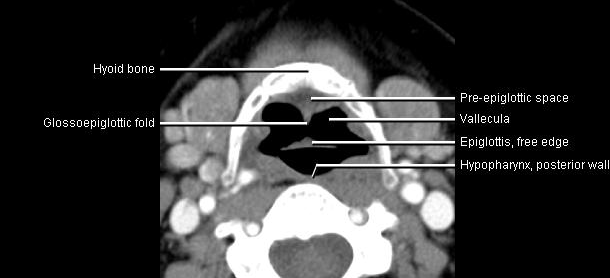
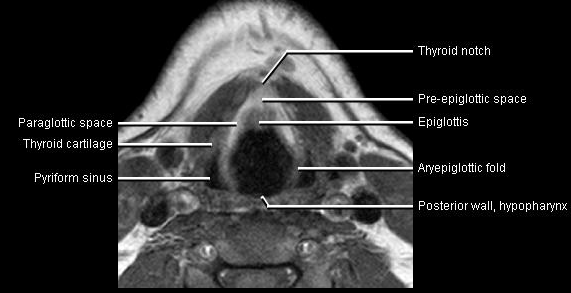
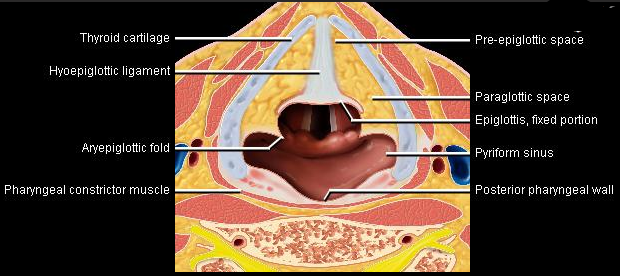
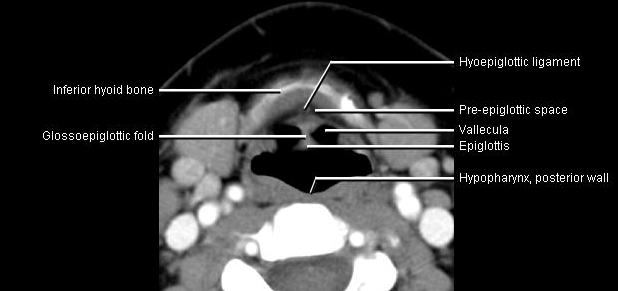
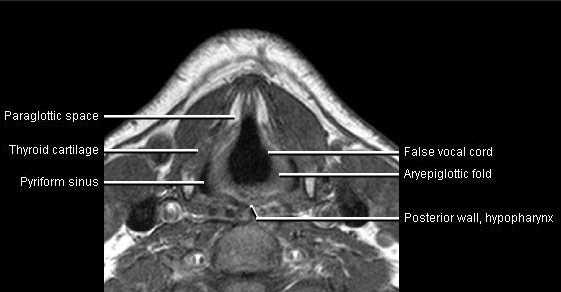
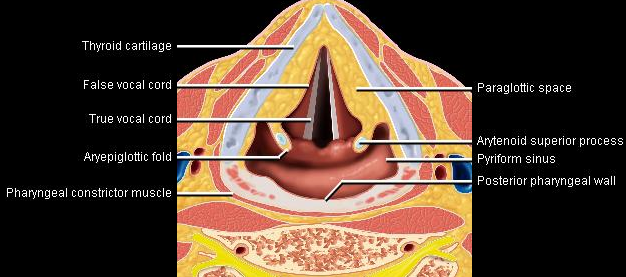
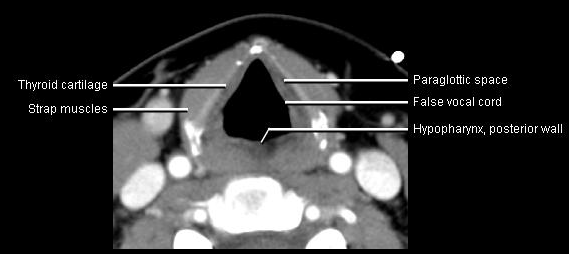
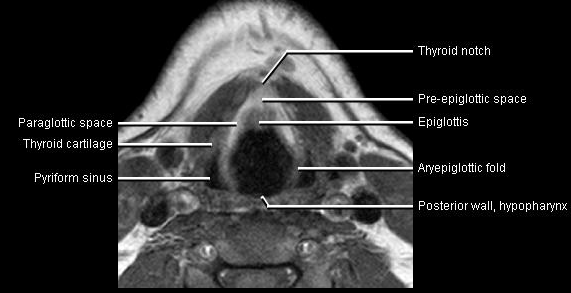
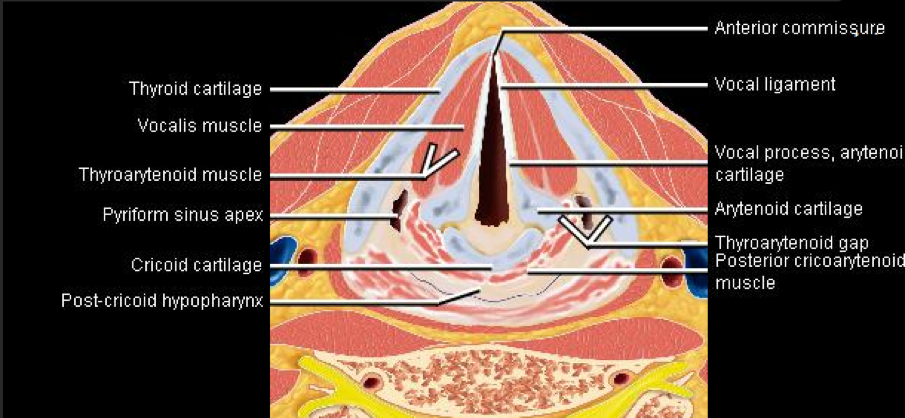
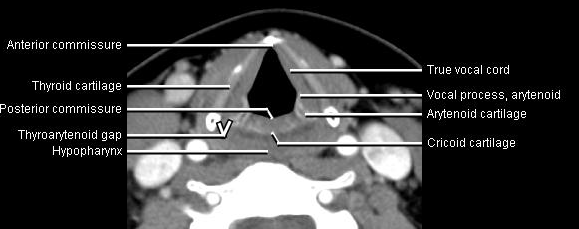
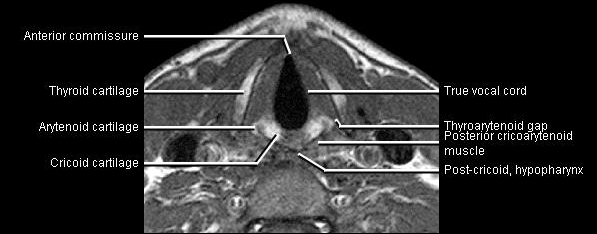
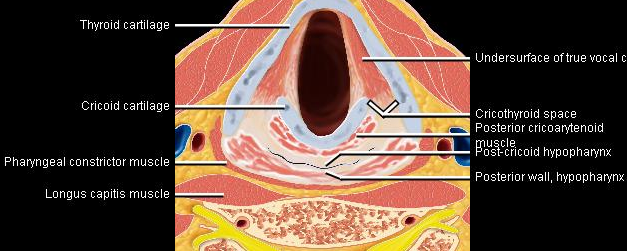
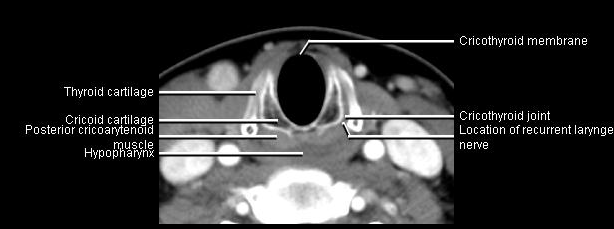
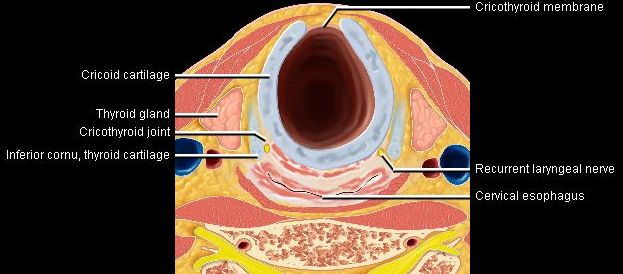
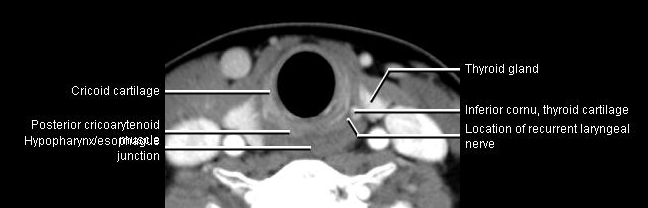
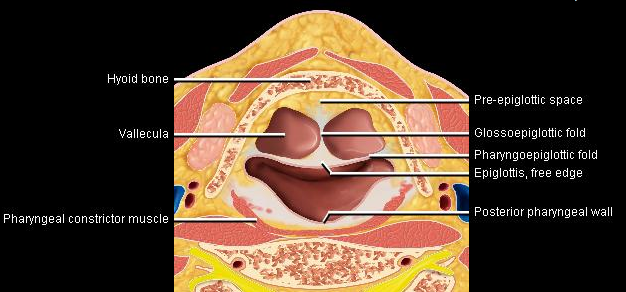
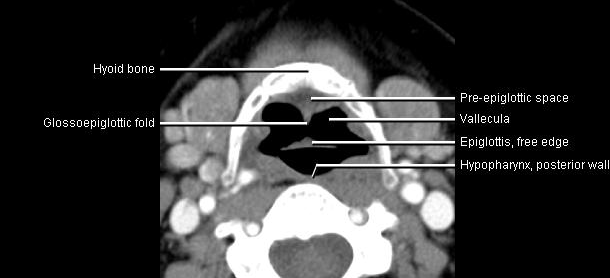
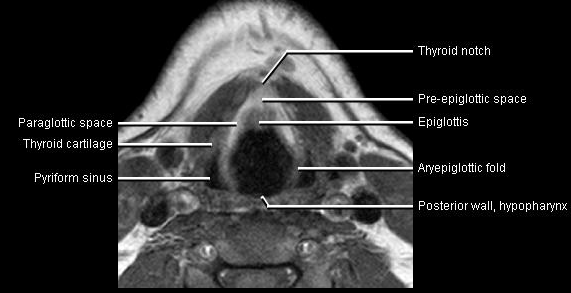
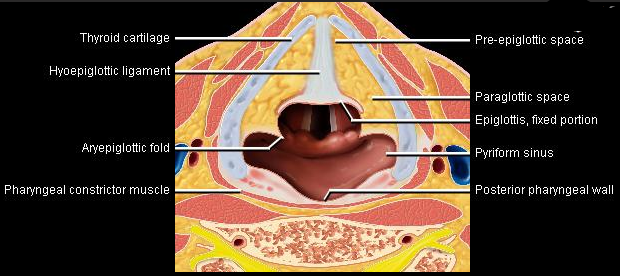
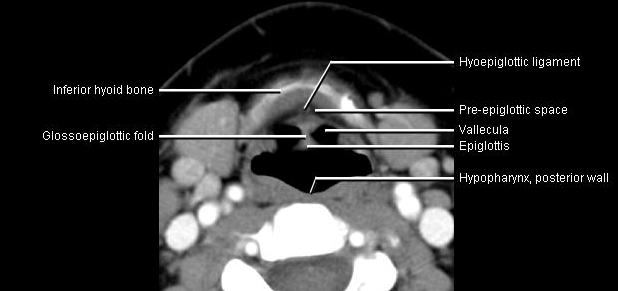
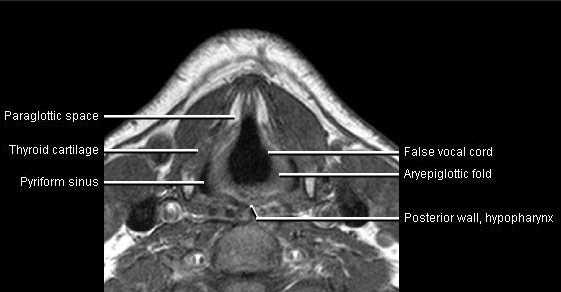
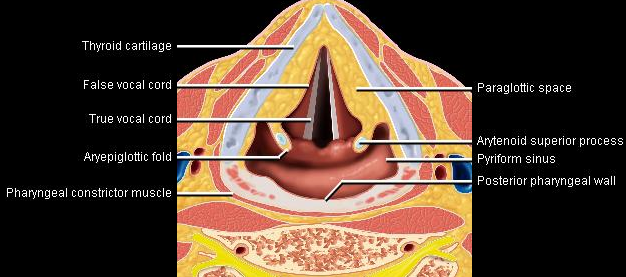
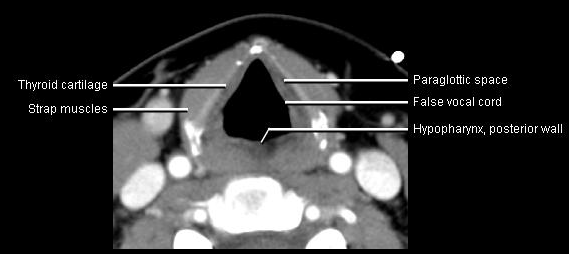
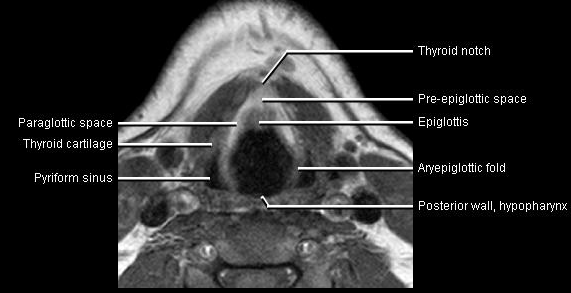
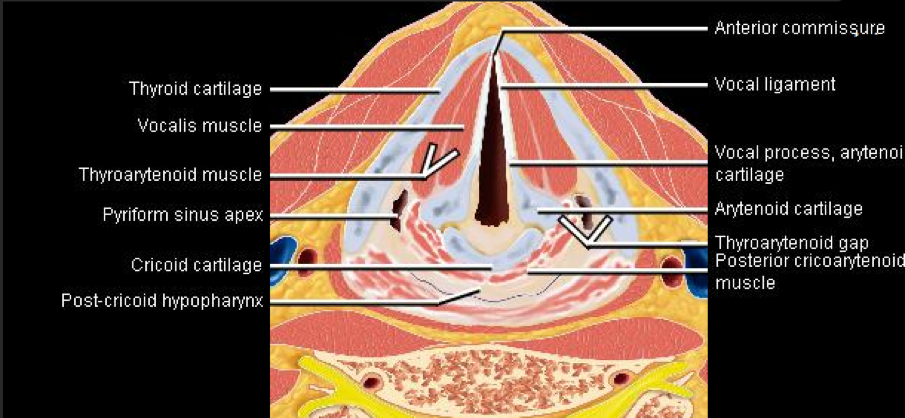
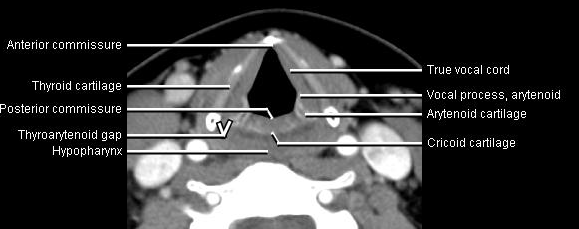
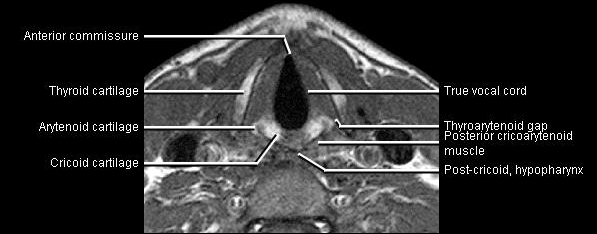
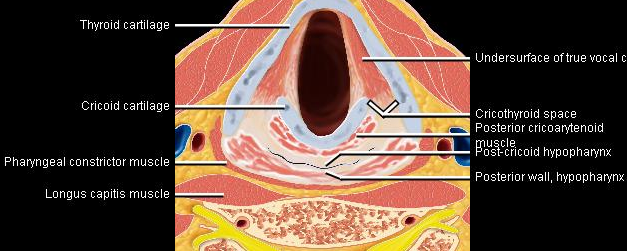
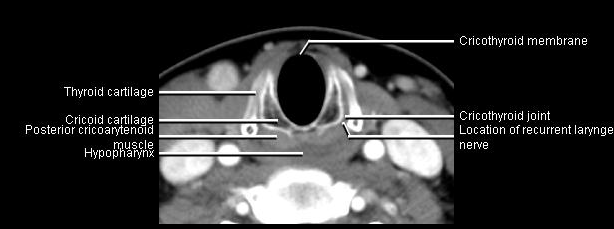
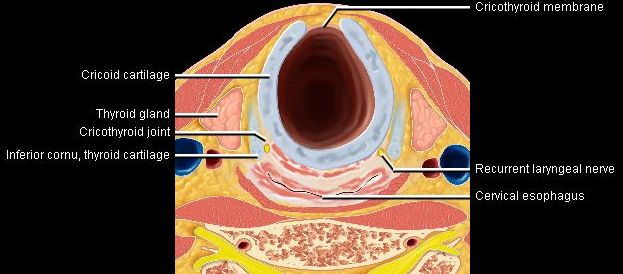
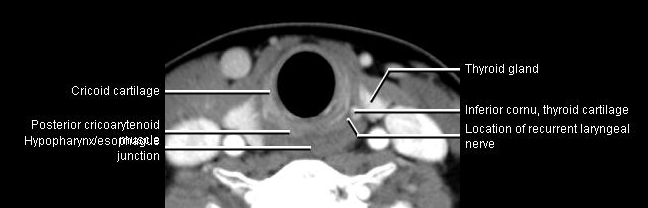
Phonation and dysphagia involve multiple coordinated structures in the larynx and pharynx. Radiation induced dysphagis appears to be related to dose to the phyaryngeal constrictor muscles and specific regions of the supraglottic and glottin larynyx.
Speech is impacted by doses to the epiglottis, base of tongue, aryepiglottic folds, false vocal cords upper esophageal sphincter and cricoid cartilage.
| Anatomy | CT | MR |
|---|---|---|
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
|
 |
 |
The mean laryngeal volume receiving > 50 Gy was a predictor of laryngeal edema. Vocal functions are usually well preserved with doses of 60 - 66 Gy. Dornfeld found a strong correlation between speech quality and dose to the ariepiglottic folds, pre-epiglottic space, false vocal cords and lateral pharyngeal walls at the level of the false vocal cords. A steep decrease in dose function was noted when doses exceeded 66 Gy.
A prospective study using IMRT to reduce dysphagia with chemotherapy plus radiation demonstrated a strong correlation between mean doses and dysphagia endpoints. Aspiration was observed when:
Chemotherapy at least doubles the risk of laryngeal edema and dysfunction. The tumor itself may also cause dysfunction and severe laryngeal dysfunction may persist after radiotherapy. If this is likely, then a laryngectomy may be preferred over chemo/radiation therapy.
QUANTEC recommends limiting the mean uninvolved larynx dose to 40 - 45 Gy and the maximum laryngeal dose to < 63 Gy to 66 Gy if consistent with tumor control. They also recommend limiting the pharyngeal constrictor volume and larynx volume > 60 Gy and when possible the volume recieving to > 50 Gy which is associated with reduced dysphagia and aspiration. This must be considered in the light of potential tumor control doses required.
The primary salivary glands responsible for bicarbonate and moisture production are the parotid, submandibular and minor sailvary glands. These glands are in close proximity to many head and neck tumors or nodal metastases. At least portions will recieve substantial doses of radiation resulting in at least some dysfunction. Although there is some protection with amifostine, radiation dose limitations are important in preserving salivary function and thus, quality of life. The parotid glands are responsible for the majority of stimulated salivary production. The maintenance salivary production (unstimulated) is due to the submandibular, sublingual and small oral salivary glands.
Parotid and submandibular glands can be identified on CT imaging. Changes in anatomy do occur with regularity during radiation treatment resulting in changes in spatial position and size of parotic glands during the course of radiation. It may be necessary to replan cases in the event of significant shrinkage, which is an additional argument in favor of using real time CT imagery in the management of head and neck cancers.
Minimal reductions in salivary flow were found in several studies when doses to the whole glands were constrained with a mean dose of ≤ 10 - 15 Gy. Salivary function decreased gradually in a dose dependent fashion for doses in the 20 – 40 Gy. The gland function is substantially reduced at doses > 40 Gy. The risk of xerostomia is lowered if at least one parotid or submandibular gland can be spared. One study reported mild to no xerostomia if one gland received a mean dose of ≤ 30 Gy. Some studies note that there is some recovery of salivary function over time with longer follow up times.
Pretreatment salivary function and medications affecting salivary flow can affect outcomes. Sparing the submandibular gland can reduce the risk of both stimulated and and unstimulated xerostomia.
To avoid severe xerostomia keep the mean dose of at least one parotid gland < 20 Gy. Keep the mean parotid dose for both glands to < 25 Gy. Severe xerostomia is a long term function of 25% of baseline. With IMRT dose should be as low as reasonably achievable considering the need for target volume coverage.
The submandibular gland dose constraint of < 35 Gy may reduce the severity of xerostomia.