Esophagus
Anatomy
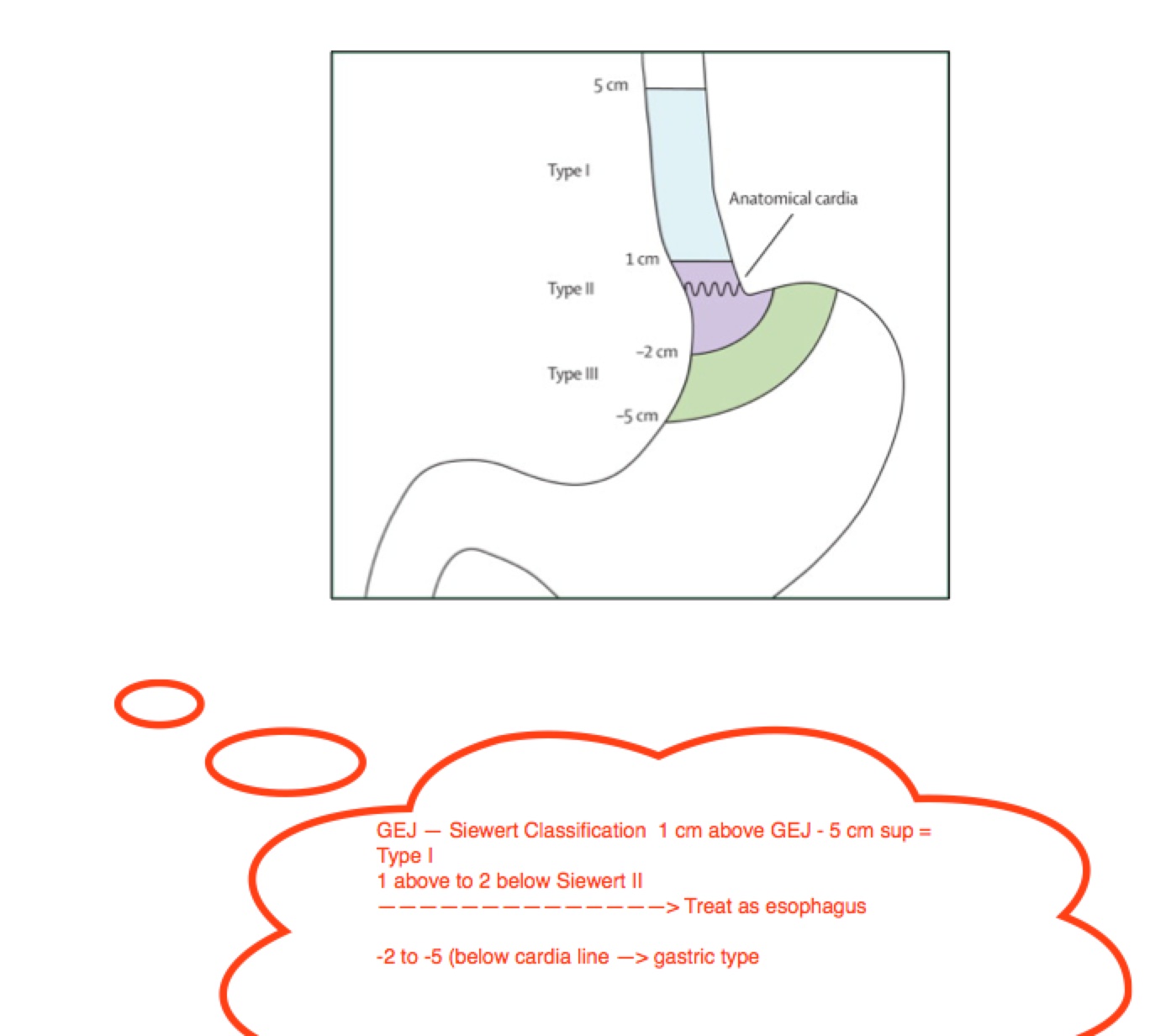
The esophagus is divided into cervical esophagus originating at the larynx, mid-esophagus in the upper thorax, and distal esophagus to the GE junction. The anatomy is defined by the Siewert's Classification, designated by 1 cm above GEJ to 5 cm above GEJ and extending distally to 2 cm below the GEJ. Below the cardia line from 2 cm to 5 cm below GEJ, is treated as Gastric disease.
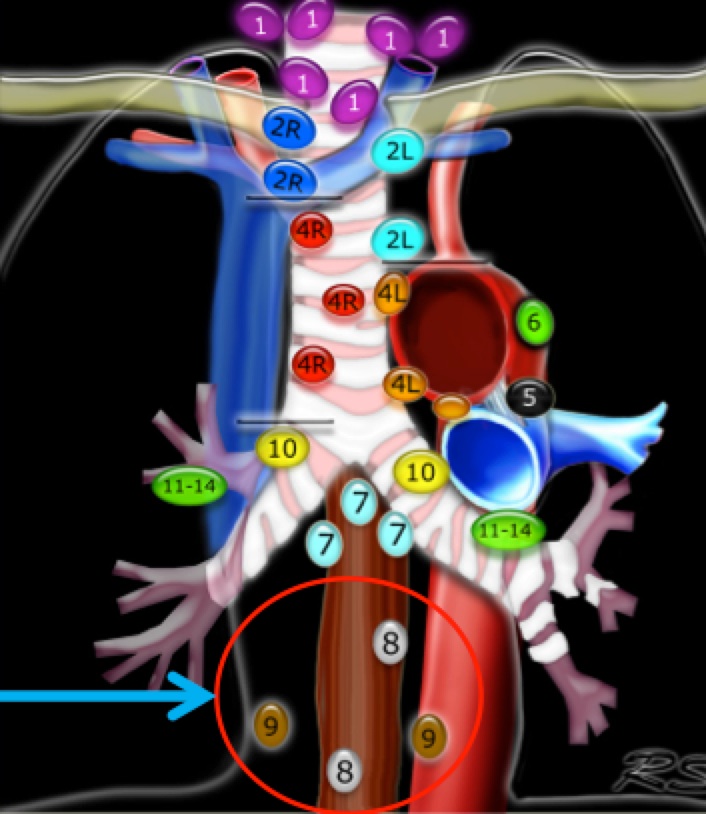
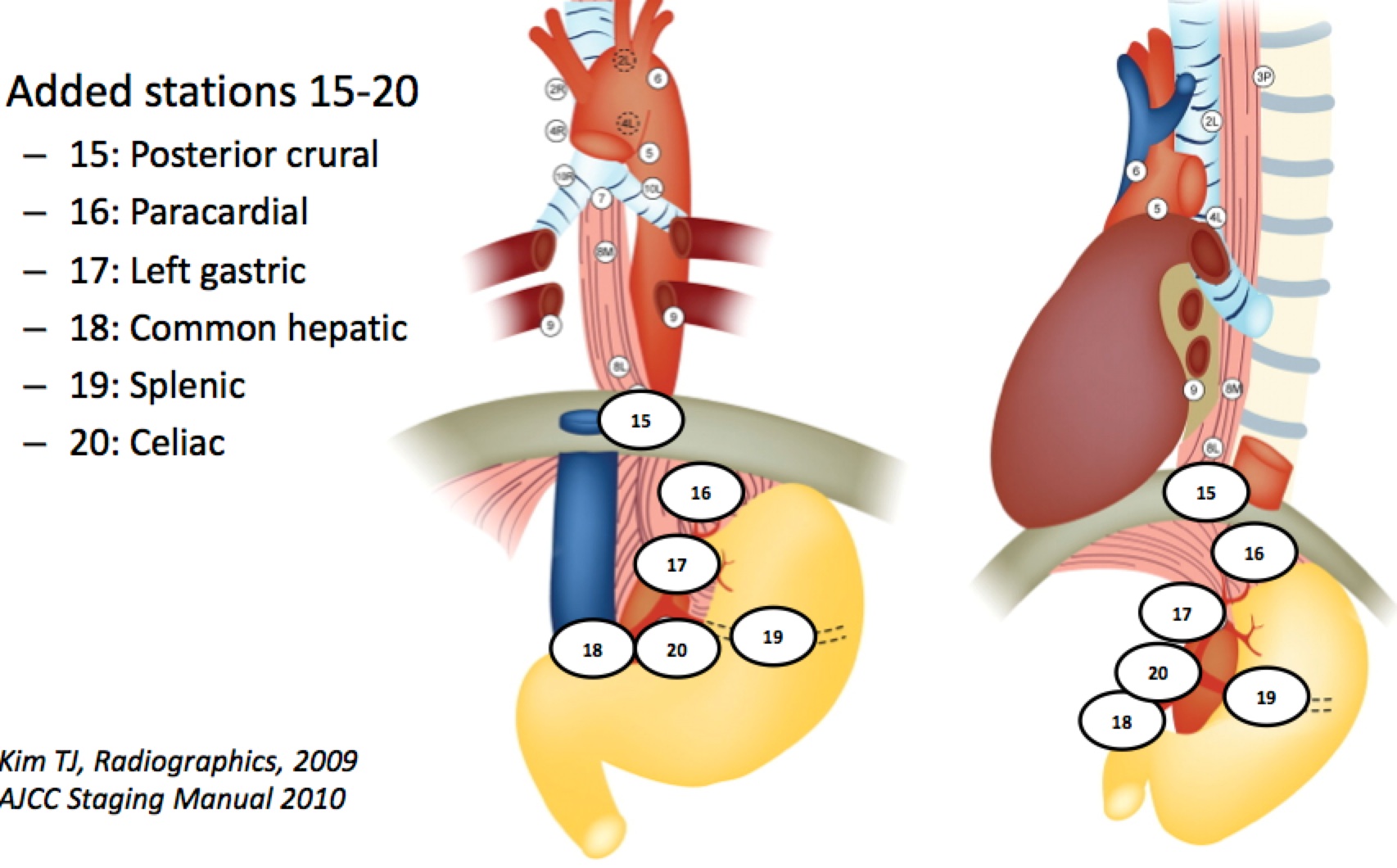
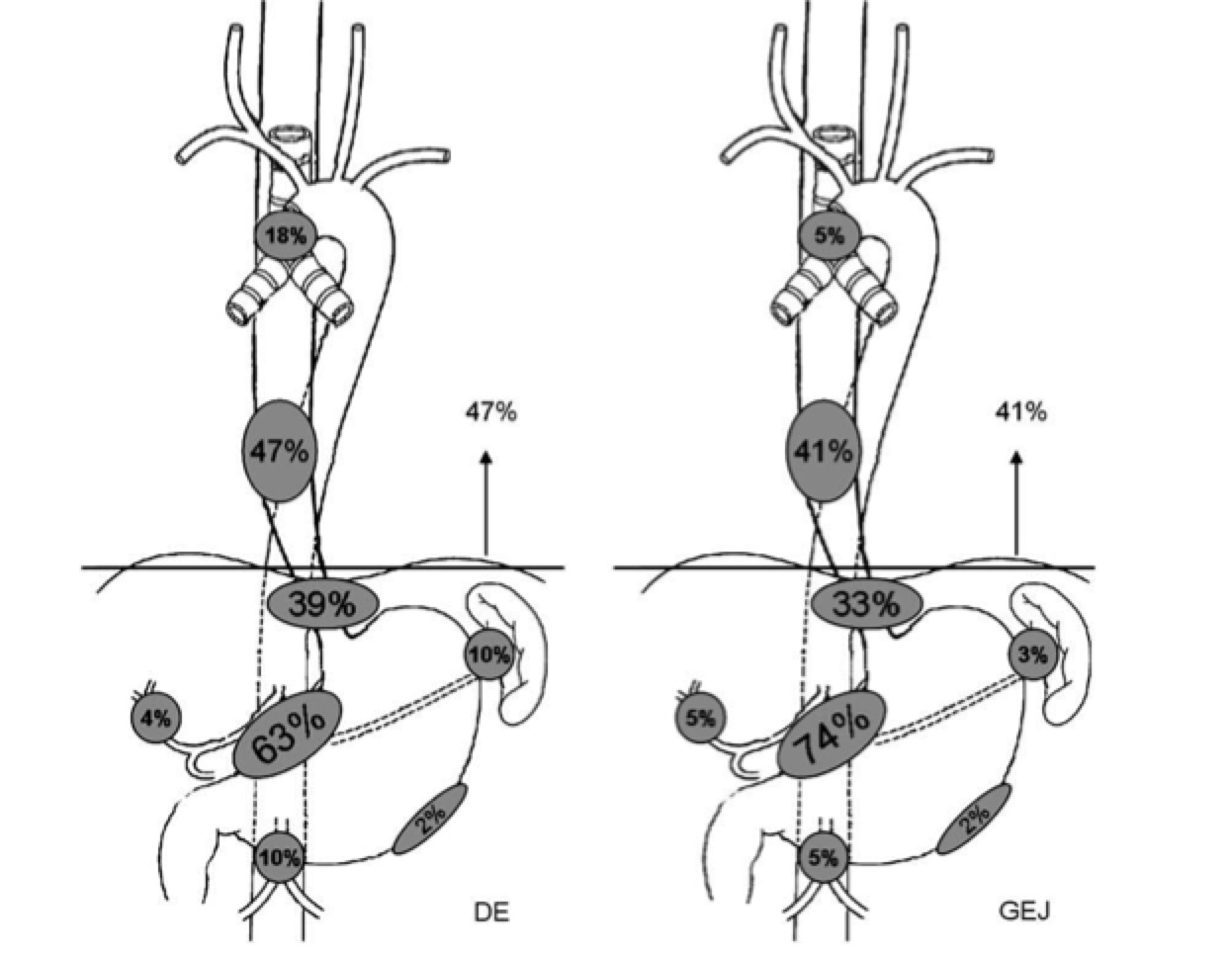
The nodal drainage basins include the supraclavicular nodes for proximal esophagus lesions, paraesophageal nodes for mid-esophagus and celiac axis nodes.
 |  |
 | |
Abraham Wu has produced a consensus atlas for esophageal cancers for use in IMRT (and 3D CRT) volumes to be covered. This is in press and can be found here (Wu et al, IJROBP 2015; doi: 10.1016/j.ijrobp.2015.03.030)
Epidemiology
Esophageal adenocarcinoma is risking with a 2.5 x increase between 1973 and 1992.
Pathology
Natural History
Clinical Workup and Evaluation
The general workup for esophageal cancer is a full H&P, blood chemistry and hemoglobin to insure chemotherapy is tolerated. Then endoscopy with endoscopic ultrasound for tissue diagnosis, followed by PET/CT or CT chest abdomen and pelvis to complete staging workup.
General Management and Treatment
Generally Esophageal cancers have been managed with neaodjuvant chemotherapy followed by surgery. Surgery is associated with a significant (up to 7%) mortality. The FFCD 9102 trial showed no difference in OS, with higher surigcal mortality at 9% v. 1%, (Bedenne, JCO, 2007).
Presently, neoadjuvant chemotherapy plus radiation followed by surgery is the standard of care. For very early disease, surgical management with endomucosal resection is used. For more advanced disease, surgical R0 resections are achieved in 60% with a 5 year OS of around 20%There is a shift away from CDDP+i5FU toward carboplatin/taxol with concurrent radiaiton. The standard radiation doses are 50.4 Gy at 1.8 Gy/fraction. There is a reduced dose study that demonstrated in surgical cases 41.4 Gy was a reasonable dose reduction, provided surgery was an option for treatment. Walsh,(1996) used noeadjuvant chemo-RT (CDDP/5FU + 40 Gy in 15 fractions) followed by surgery. Walsh's surgical arm was underperforming with an 11 month median survival, but CRT matched other trials, including Susan Urba's 45 Gy BID trial.
The CALGB 9781 trial used CDDP+5FUx2 + 50.4 Gy followed by surgery, compared to surgery alone. The OS5 was 39% in the neoadjuvant chemoRT arm, and 16% in the surgical arm. Median survival was much worse in the surgery only arm at 1.8 years v. 4.5 years. This was confirmed by the CROSS trial which included GEJ tumors with OS5 of 47% v. 34% in the neoadjuvant arm and MS 49 months v. 29 months. CALGB used 41.4 Gy which showed a definite benefit of neoadjuvant chemo-RT, even at reduced RT doses. Local recurrences were 5% in the target volume, 2% at the margin and 6% outside the treated volumes.
The POET trial looked at neoadjuvant induction chemotherapy followed by surgery v. chemo → chemoRT → surgery. RT was 30 Gy, and chemotherapy was CDDP/5FU/leucovorin induction and CDDP/VP16 concurrent. This trial had poor accrual and closed early, with improved pCR in the concurrent chemo-RT arm. There does not appear to be a role for neoadjuvant induction chemotherapy.
ECOG looked at Neoadjuvant CRT with Oxaliplatin and demonstarted an unacceptable toxicity rate with a 22% ARDS operative mortality and 32% mortality rate with 45 Gy + oxaliplaitn/5FU, cetuximab. These deaths did not appear to be associated iwth RT or IMRT regimens.
CALGB 80803 randomized a phase II trial to look at PET response and chemotherapy. T3/4 or N1 disease was randomized to induction chemotherapy: FOLFOX6 or Carbo/taxol and rescanned after Day 36-42. For PET responders (≥ 35% SUV decrease), the initial chemotherapy was continued with the addition of radiation to 50.4 Gy at 1.8 Gy/fraction. For non-responders, the chemotherapy arm was crossed over and RT was given. Everyone got surgery.
Radiation Therapy Treatment Planning And Techniques
Several trials and dose/chemotherapy regimens have been investigated. For patients with definitive therapy without or not candidates for surgery, the dose should be 50.4 Gy. If surgery is definitely planned, then a reduced dose may be acceptable to meet normal tissue constraints. RTOG 1010, the most current RTOG esophageal trial uses the same radiation in both arms, and does permit IMRT or 3D-CRT.
For workup and treatment planning, the simulation is supine on the wingboard with arms overhead. IV and oral contrast to enhance the esophgus is used and CT images are taken at 2.5 mm cuts. These are fused with the diagnostic PET/CT for delineation of target volumes. If the GEJ region is involved, it might be useful to use 4DCT for respiratory motion studies.
Volumes
- GTVp
- the primary esophageal tumor based on EUS/endoscopy, CT and PET/CT
- CTVp
- —CTV expansion on GTV. The expansion is dependent on imaging. There are two expansions, a superior-inferior expansion on the tumor which is either 5 cm for non-4d imaging, or 4 cm if respiratory imaging is used.
- —If 4dCT imaging is used, then an ITV should be constructed from the respiratory binning and a 4 cm superior-inferior expansion should be used.
- — Radial expansions should follow the esophagus, at 1-1.5 cm radially to cover para-esophageal nodes.
- CTVn
- This is the nodal at risk definition which includes the celiac axis in the distal/mid esophagus and GEJ, and supraclavicular/low neck nodes in the proximal esophagus.
50.4 Gy is delivered to the PTV
Radiation fields are used to avoid cord, kidneys, heart, lungs, and liver. Most commonly is the "Mercedes" fields with an AP or PA field and a pair of oblique fields. Sample fields and gantry angles are given below:
| Field | IEC gantry |
|---|---|
| LPO | 155 |
| RPO | 205 |
| AP | 0 |
| PA | 180 |
| RAO | 325-330 |
| LAO | 70-80 |
IMRT fields may use additional fields, but it is generally better to constrain them to 5 fields, to insure that minimal low dose lung exposure takes place to reduce toxicity.
Dose limitations for the esophagus, in order of imprtance:
| Organ | Constraints | ||
|---|---|---|---|
| Spinal Cord | Dmax 45 Gy | ||
| Lung | V20 < 20% | V10 < 40% | V5 < 60% |
| Heart | V40 < 30% | V30 < 30% | Dmean < 25 Gy |
| Liver | Dmean < 25 Gy | V30 < 30% | |
| Kidneys (R&L) | Dmean < 18 Gy | V18 < 33% |
Outcomes, Patterns of Failure, Prognostic Indicators
Studies discussed above had shown an OS5 around 40% with better outcomes in early PET responders.
Side Effects and Complications of Treatment
More recent data from MDACC has shown that cardiac dose sparing results in better outcomes. IMRT reduced the mean heart dose from 28 to 23 Gy, reduced the V30 from 61% to 24.8% and reduced teh mean RCA dose to 24 from 36 Gy.
Grade 3 esophagitis was reduced, as was nausea. Overall survival was improved in short follow up from 52.4% at 5 years v. 31.3% at 5 years. Median survival was also improved form 24 months to 36 months when using IMRT.
What is most significant is that cardiac deaths dropped substantially, as did other deaths. What is not clear is the techniques used in the comparison 3D-CRT fields. Lateral fields appear better on DVH diagrams, but can increase lung toxicity.