Primary CNS Lymphoma
Epidemiology — Natural History — Pathology
Primary CNS lymphoma is a non-Hodkin's Lymphoma restricted to the CNS. It is localized to the brain, spinal cord, meninges and eye. PCNSL accounts for < 3% of all CNS primaries. It occurs in immunocompromised (HIV, Post Transplant) populations and immunocompetent populations. Immunodeficiency is the only known risk factor. Immunocompetent patients present in their 50's or 60's, and immunocompromised patients present earlier in their 20s and 30s. The majority of CNS lymphomas are B-cell derived intermediate or high grade lymphomas that are indistinguishable from extra-CNS high grade NHL. EBV and HIV/AIDS are predisposing conditions. Lower grade tumors tend to be T-cell derived.
The majority (in immunocompetent patients) present with one or multi-focal mass lesions primarily in the frontal lobes, corpus callosum and deep periventricular brain structures. Diffuse involvement is invariably present. Patients usually present with cognitive dysfunction or personality change. Other CNS symptoms are rare. Symptoms are usually progressive over weeks to months prior to diagnosis.
Clinical Workup and Evaluation
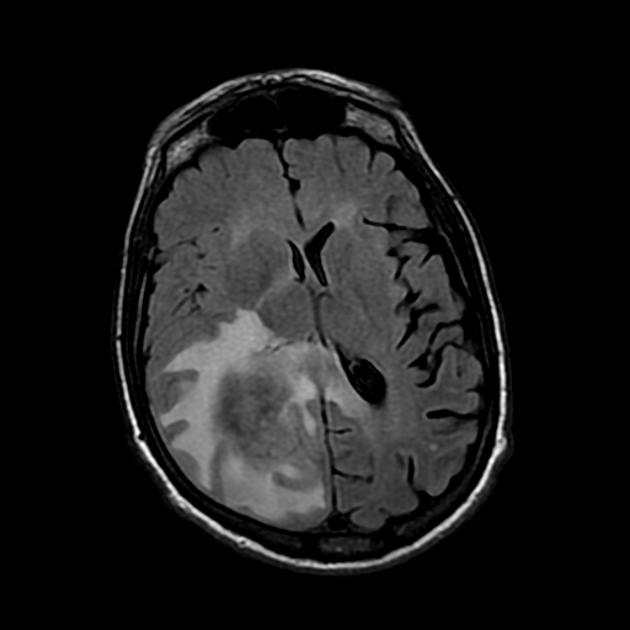
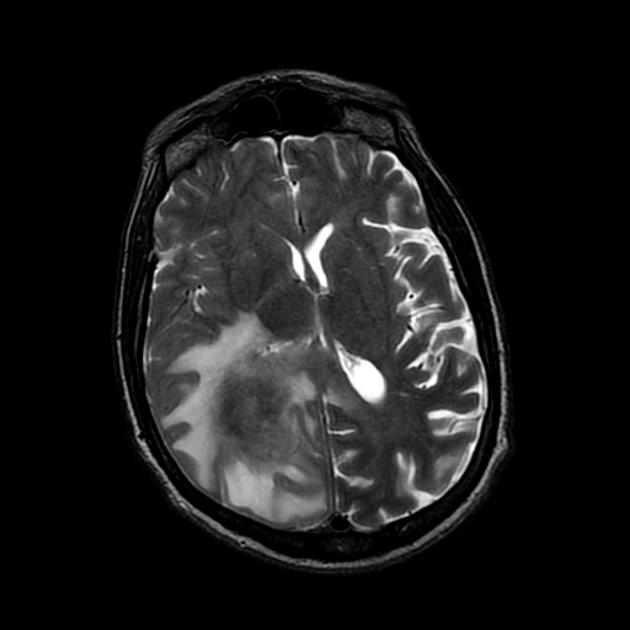
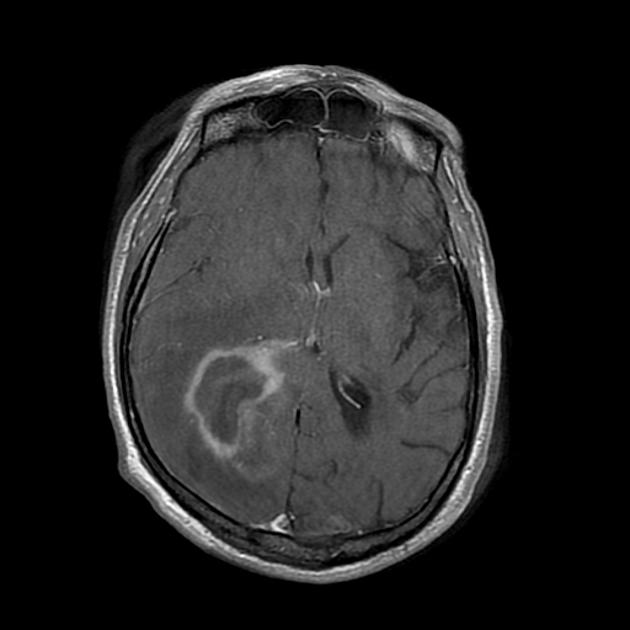
A detailed history and physical evaluation with particular attention to time course and nature of symptoms, followed by an MRI of the brain is the usual initial workup. The T1 MRI shows a hypointense or isointense lesion, and T2/FLAIR shows variable surrounding edema. T1/Gad shows homogenous enhancement without ring enhancement and lacking central necrosis. Ring enhancement occurs more often in immunocompromised patients.
Histologic determination is essential to proper treatment selection. If PCNSL is suspected, further workup is necessary to obtain tissue. An eye exam (slit lamp) to look for intra-ocular masses/lymphoma, spinal tap if safe with flow cytometry, and brain biopsy if CSF and eye exams are negative. A stereotactic biospy (least invasive approach) is the best approach. Extensive surgery does not improve survival. Corticosteroids should not be administered unless absolutey necessary until after the brain biopsy is completed or tissue diagnosis is confirmed. If corticosteroids are given before biopsy, a false negative biopsy is possible.
If a CSF tap is obtained and is positive, or there are symptoms of spinal cord involvement or HIV positive, then the spine should be imaged. Some recommend a testicular ultrasound and some recommend a bone marrow biopsy. If B-signs are present, a CT of the chest abdomen and pelvis should be done to look for other sites of disease. Some advocate a PET/CT, but presently, in the United States, there are increasing financial barriers to PET/CT imaging (2014).
Ocular involvement is present in 25% as is leptomeningeal involvement. Ocular involvement may present as uveitis. Laboratory studies should include: CBC, comprehensive chemistry (including LDH), and HIV serology.
Imaging
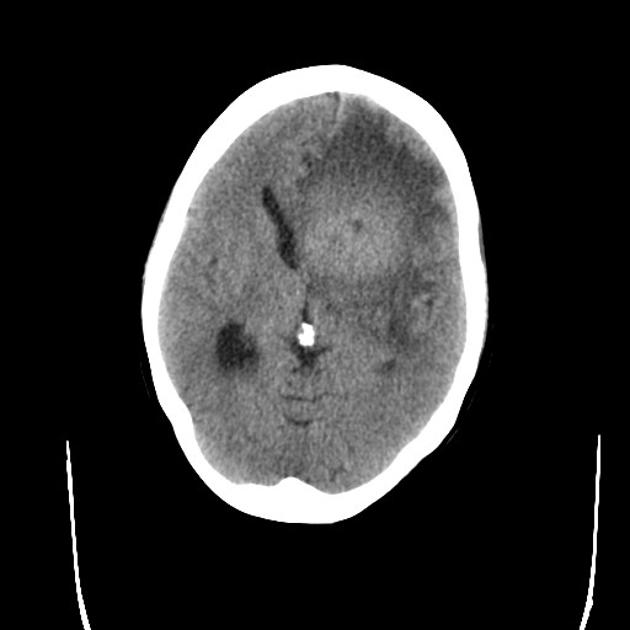
CT Imaging
CT images are hypointense. Hemorrhage is uncommon. Multiple lesions are more common in HIV+ patients.
 |  |
MRI
- T1/no contrast — hypointense w.r.t. white matter
- T1+gad
- high grade tumors show strong homogenous enhancement
- lower grade tumors show less strong homogenous enhancement
- T2 — low grade tumors tend to show more enhancement, higher grade, less enhancement
- MR-spect: large choline peak, lactate peak sometimes seen.
 |  |
 |
General Management and Treatment
Radiation Therapy Treatment Planning And Techniques
Surgery is limited to providing tissue for diagnosis. This is best acheived by stereotactic biopsy. Resection offers no benefit for local control or survival. Primary CNS lymphoma responds dramatically to corticosteroids, so tissue should be obtained, if possible before starting steroids.
PCNSL is exquisitely sensitive to radiation and chemotherapy. WBRT is thought to be more effective than focal radiaotherapy due to the extensive microscopic infiltration of the disease. Whole Brain Radiation therapy may be omitted in teh primary treatment setting in patients treated with chemotherapy with a complete response. If WBRT is offered, dose should be 1.8 Gy/fraction to 23.4 Gy after CR to chemotherapy. For less than complete response, radiation should be considered. The optimal dose (per Perez and Brady 6th ed., p 671.) is 45Gy - 50 Gy delivered to the residual disease site only. The NCCN comments that the lower doses are less toxic and may be as effective.
Whole brain radiation therapy is used as a consolidation therapy after chemotherapy, particularly in patients younger than 60. Patients older than 60 are at risk for treatment related Chemotherapy generally consists of high dose rate methotrexate of 1 - 8 g/m2 rapidly administered to overcome the blood-brain-barrier. This is the only agent that has shown advantage over WBRT alone. If CSF is positive for disease, then an Ommaya reservoir may be needed and direct intrathecal MTX may be required. Induction chemotherapy consists of high dose rate MTX, plus deferred RT, with Retuximab or retuximab and temozolomide.
For patients who are not candidates for chemotherapy, WBRT to 24-36 Gy followed by a boost to gross disease to 45 Gy should be considered. All doses delivered at 1.8 Gy/fraction.
Outcomes, Patterns of Failure, Prognostic Indicators
Important prognostic indicators from a Memorial review include :
- RPA Class I (MSKCC): age < 50 years, Median survival 8.5 years
- RPA Class II (MSKCC): age > 50 years and KPS ≥ 70, Median survival 3.2 years
- RPA Classs III (MSKCC): age > 50 years and KPS < 70, Median survival 1.1 years
The International Extranodal Lymphoma Study Group found the following adverse prognostic indications:
- age > 60
- ECOG PS > 1
- elevated LDH
- high CSF protein
- deep regions of the brain involved.
Side Effects and Complications of Treatment
There is a very high rate of serious CNS sequalae when radiation is given in close proximity to methotrexate. This includes loss of continence, dementia, and ataxia. These sequalae are much higher in patients older than 60. The risk is greatest in patients ≥ 60 and when methotrexate is administered concurrently or subsequent to radiation therapy. In a phase II trial, the toxicity rate was 100% in patients age 60 and older at 24 months while the toxicity rate in those younger was 30% at 96 months.