Ependymoma
Epidemiology and Pathology and Natural History
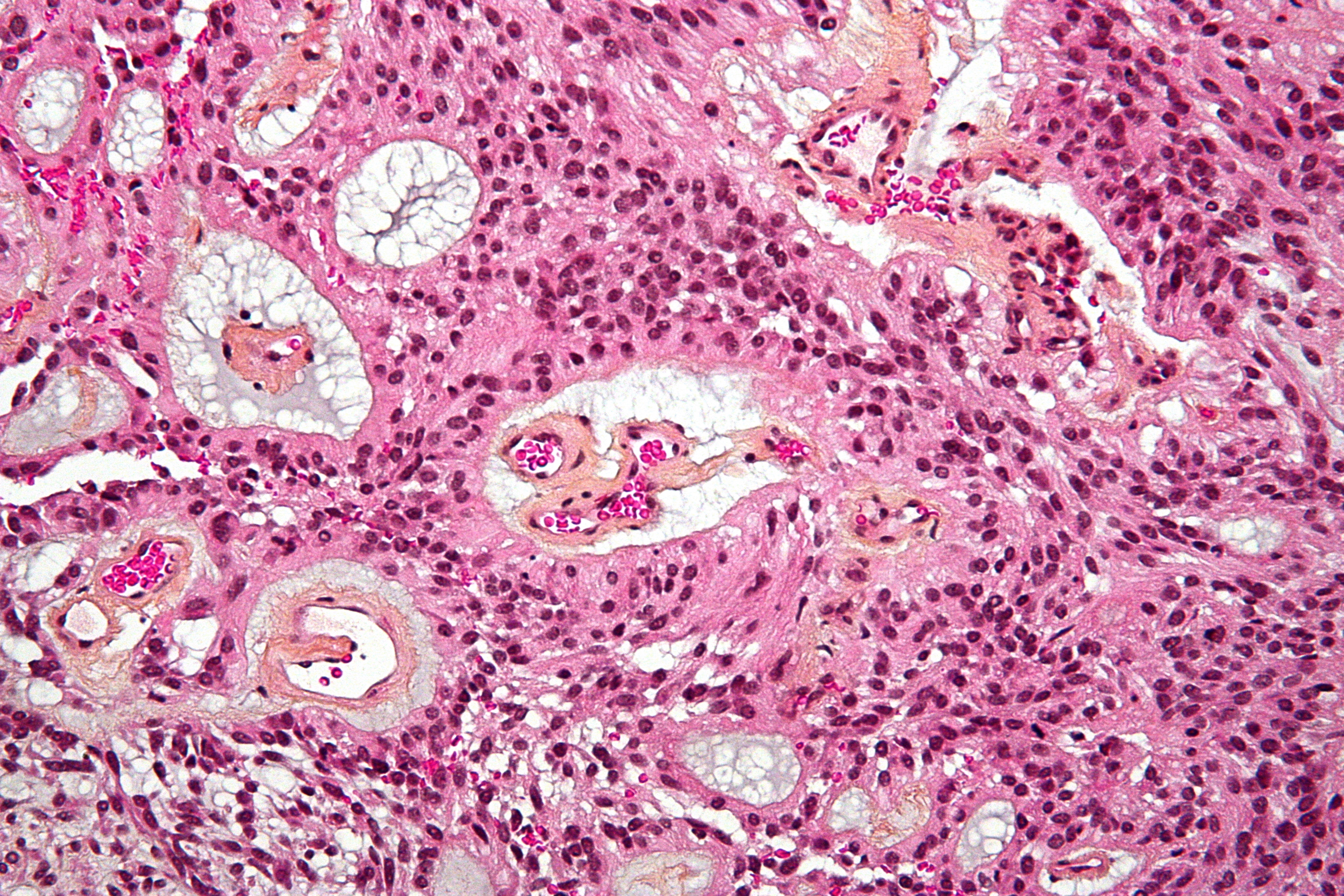
Ependymoma accounts for less than 2% of all adult brain tumors. Rosette formation is a hallmark of ependymoma with increased cellularity, cytological atypia and microvascular proliferation which suggests ependymoma.
 |
Adult ependymomas generally occur in the spine (75%), unlike pediatric ependymomas which arise intracranially. The usual clinical presentation is a sensory deficit. They may expand locally, track along ependymal spaces, or occasionally dissminate through CSF spread. The predominant pattern of failure is local relapse, even in anaplastic disease.
There are 4 grades of ependymoma:
| WHO Grade | Description |
|---|---|
| WHO Grade I | myxopapillary ependymoma |
| WHO Grade II |
|
| WHO Grade III |
|
Clinical Workup and Evaluation
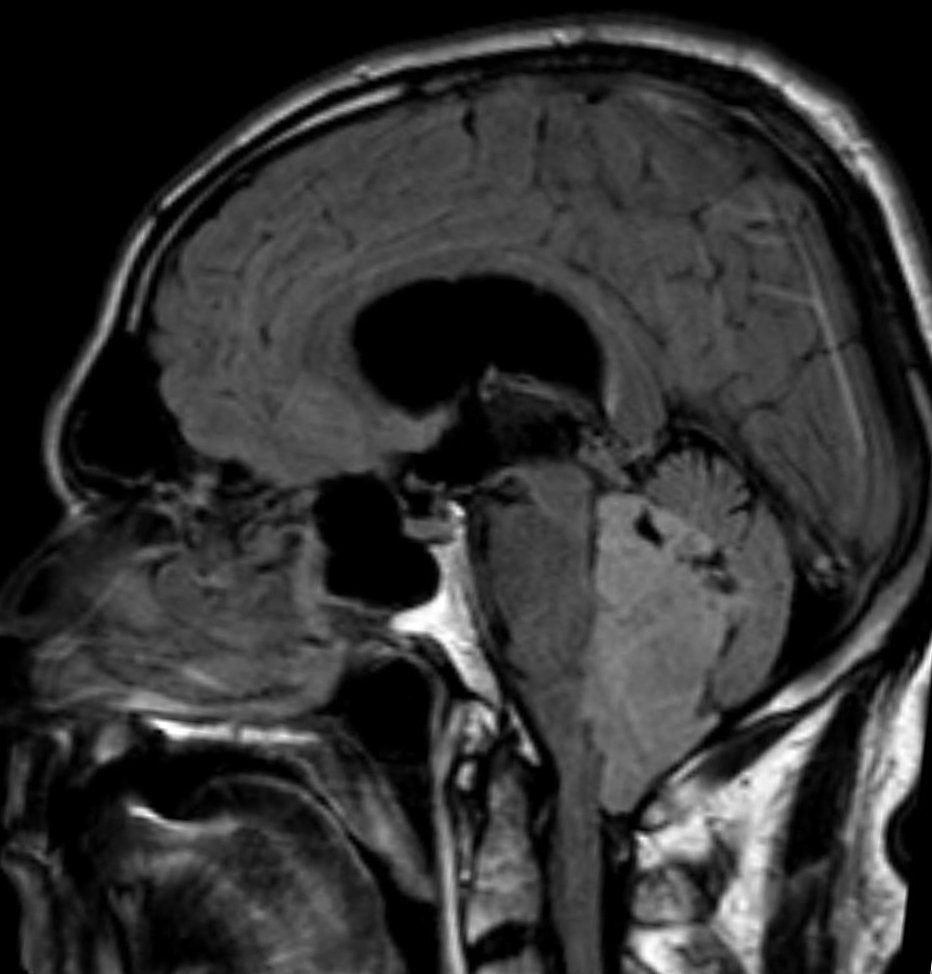
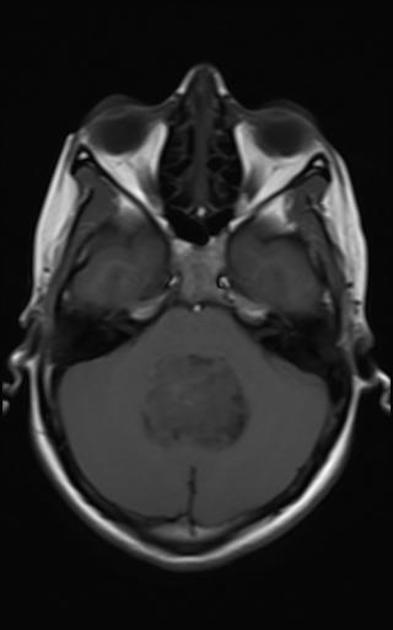
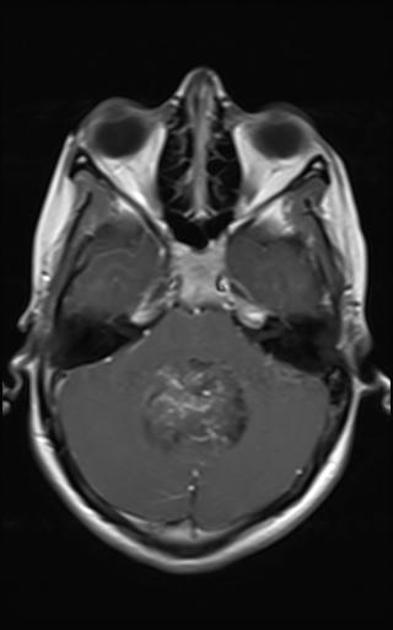
Imaging is the usual initial workup followed by surgery or biopsy for tissue diagnosis. Surgery alone may be adequate in selected patients based on the results of pediatric series. The usual standard of care for adults is post-operative radiation. Post operative workup includes an MRI of the CNS axis with contrast, consider CSF analysis. If CNS imaging is not obtained before surgery, then a waiting period of about 3 weeks should be met before additional imaging to insure artifacts from surgery do not interfere with the study.
The initial work up should be an MRI with contrast or alternatively a Contrast Enhanced high resolution CT of the brain. Once imaging is obtained then a decision can be made concerning the extent of surgery. Ideally, the surgery should be a gross total resection. If this is feasible, then proceed to surgery for gross total resection. Otherwise, a sub-total resection or stereotactic biopsy will obtain tissue for definitive diagnosis. A postoperative contrast enhanced MRI of the brain should be obtained within 72 hours of surgery (POD 1), the spine MRI should be delayed by 3 weeks to insure there are no surgical artifacts. CSF fluid must be analyzed in the case of anaplastic ependymoma (Grade IV), otherwise it should be considered. If the MRI of the spine is negative, then proceed to LP. The LP should be delayed at least 2 weeks to avoid false positive associated with surgery and, in the case of a posterior fossa mass, an LP should be avoided.
| Axial T2 | Sagital FLAIR | |
|---|---|---|
 |  | |
| Axial T1 | Axial T1 Gad | Axial T1 Gad/fat sat |
 |
 |
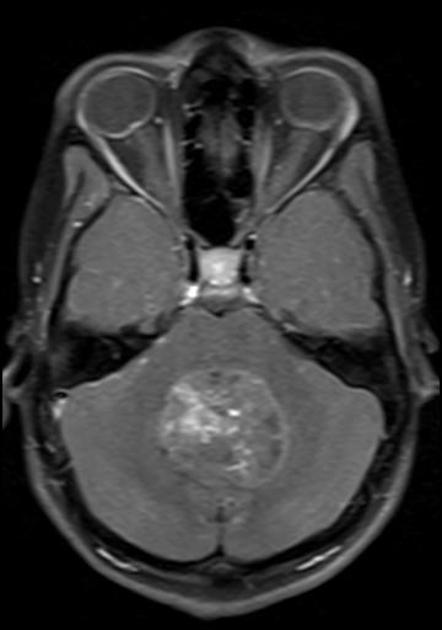 |
For a detailed discussion of ependymoma imaging see Radiopedia for an excellent discussion on ependymoma imaging by Weerikoddy and Galliard.
MRI Brain
-
T1
- solid portions of ependymoma typically are isointense to hypointense relative to white matter 7
-
T2
- hyper intense to white matter
- more reliable in differentiating tumour margins than non-contrast T1-weighted images (but less reliable than contrast enhanced T1)
-
T2* (e.g. SWI)
- foci of blooming from haemorrhage of calcification
-
T1 C + (Gd)
- enhancement present but heterogeneous
- enhancement with gadolinium is useful in differentiating tumour from adjacent vasogenic oedema and normal brain parenchyma
-
DWI / ADC
- restricted diffusion may be seen in solid components especially in anaplastic tumour
- diffusion should be interpreted with caution in masses with significant haemorrhage or calcification
Careful examination of the entire neuraxis is required to assess for the presence of CSF seeding.
Summary of Clinical Workup
- Initial Signs and symptoms point to CNS process, localizable to brain → MRI Brain.
- Brain mass found,suspicious for ependymoma (4th ventricle, supratentorial)
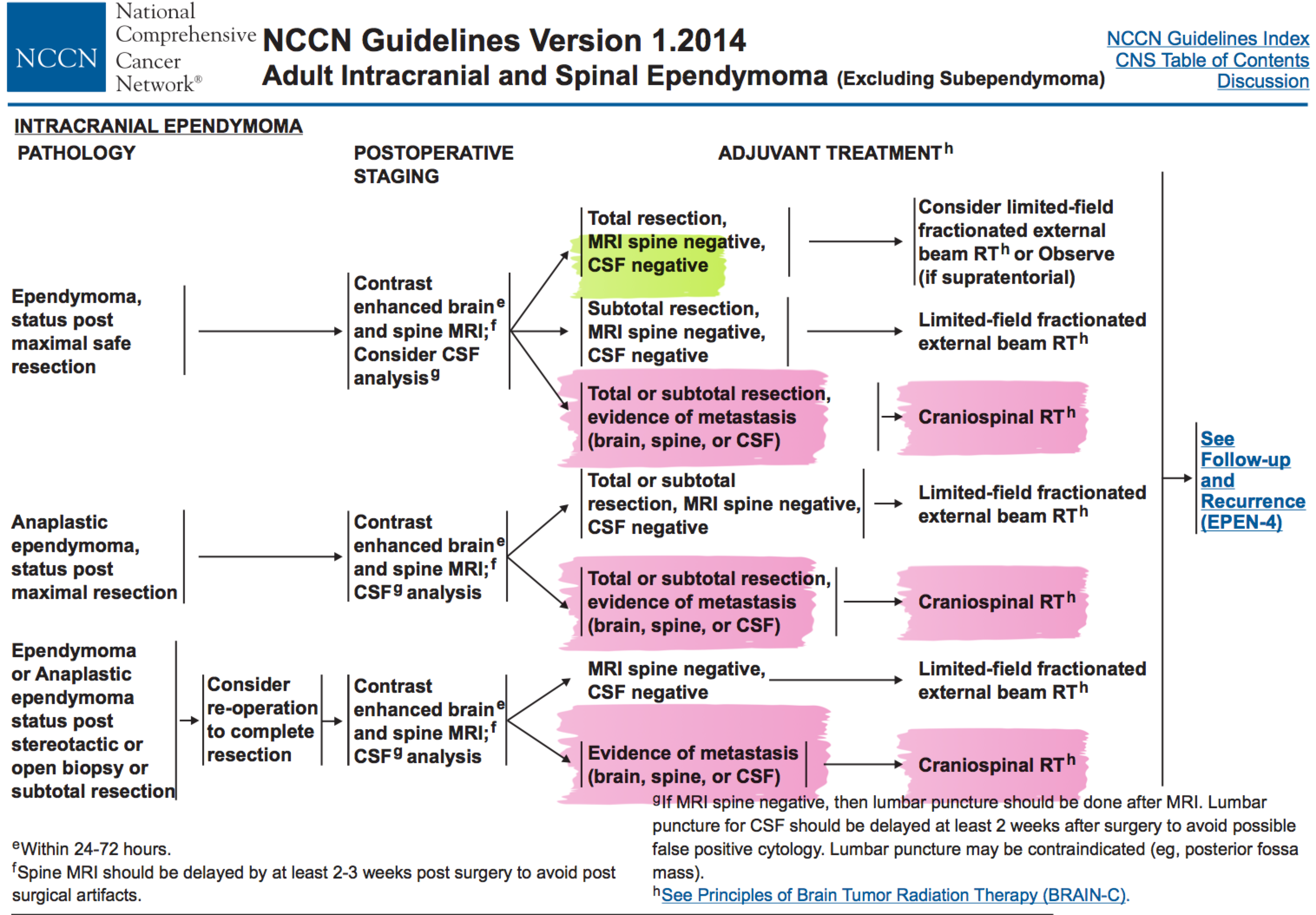
General Management and Treatment
Surgery is the initial treatment of choice. Maximum possible surgical resection is indicated. Incomplete surgical resection is a worse prognostic indicator. Post-operative radiation is indicated and studies have shown that the predominant pattern of failure in non-metastatic disease is local, based on pediatric experience. AC Paulino reported 9 patients who received local radiation only, to the tumor bed plus 2 cm margin, only two failed, and those two within the tumor bed and irradiated area. There were no failures in the posterior fossa outside of the tumor bed. For most patients with non-metastatic disease, the radiation target volume is the tumor bed, residual disease + 1.5 cm margin, paying careful attention to the degree of infiltration patterns and possibility of spread down the cervical spine. For very localized Grade I disease, observation may be sufficient, but generally, in ependymomas, post-operative radiation is offered. Recurrence portends a very bad prognosis.
Radiation Therapy Treatment Planning And Techniques
Localized (non-metastatic disease)
The current recommendations for patients with ependymomas are limited field radiation if the MRI and CSF are negative. Patients with postive neuroaxis spread (positve MRI or CSF) should be treated to the cranio-spinal axis. The recommended dose varies (Perez: 40-45 Gy, NCCN, UCSF 36 Gy). 36 Gy appears to be more prevelent. Gross disease should be boosted to 54 Gy to 60 Gy. Pediatric doses are
Supratentorial Tumors
These tumors are more common in adults. Radiation fields for non-metastatic disease are now local, limited involved fields. As discussed above, special attention should be paid to the prospect of 4th ventricle tumors spreading into the upper cervical spine. About 10%-30% spread throught he foramen magnum. The general radiation target volume for localized intracranial disease is the GTV+resection cavity + 1.5 cm, with larger margins when diffuse infiltration is suspected.
Doses to localized brain tumors is 54-60 Gy at 1.8 - 2.0 Gy/fraction.
Spinal Cord Tumors
Spinal ependymomas are treated 2 vertebral bodies above and below the visualized tumor. The lateral aspects of the field should include the nerve roots. For tumors in the sacrum, coverage should include the sacrum nerve rootswith caudal border at S4/S5 and lateral borders to the SI joints.
Dose to gross disease regions is limited to 45 Gy at 1.8 Gy/fraction.
Metastatic Ependymomas (positive CSF or positive MRI for disseminated disease)
Cranio-spinal irradiation is no longer indicated for isolated disease. It is indicated for disseminated disease, including positive CSF or imaging findings. First image the spine with MRI. If the MRI is negative, then proceed to LP and CSF collection and analysis. If the CSF is negative, then treat locally as appropriate. Otherwise, proceed to CSI.
Dose is 36 Gy to the CSI, followed by a boost to 54-60 Gy to the involved field, as described above, in the case of brain primary, or 45 Gy in the case of spinal primary.
In the case of incomplete resection, the dose does not change.
Outcomes, Patterns of Failure, Prognostic Indicators
Prognosis is relatively poor which is mainly due to tumors occuring in surgically challenging locations make complete resection difficult. Poor prognostic factors include location in the 4th ventricle, anaplastic variant and incomplete resection. As such children have a worse prognosis (both 4th ventricular location and anaplastic variant are more common in children). Overall the 5-year survival rate in children ranges from 50% to 75%.
Once recurrence has occurred prognosis is very poor, with a mortality rate of 90%.
| Group | PFS5 | OS5 |
|---|---|---|
| Adult GTR Localized | 50%-55% | |
| Adult STR localized | 0% - 25% | |
| Adult Anaplastic STR | 50% - 60% (OS) | |
| Adult Unresectable | 5% - 20% | |
| Peds GTR Localized | 50% - 80% | |
| Peds STR Localized | 30% | 60% - 90% |
| Peds ≤ 4 | 45% | 45% |
Followup
Serial imaging of the CNS axis covering the regions initially positive every 3-4 months for year 1, then 4-6 months for year 2, then every 6-12 months is recommended. If there is a recurrence, maximum safe resection → radiation if no prior radiation or consider re-irradiation. Chemotherapy can be considered (platinum, temozolomide, vp16, avastin, carmustine/lomustine) if radiation is unavailable.
Treatment Summary for Ependymomas
- Maximum safe surgical resection
- Post-operative radiation therapy is considered standard. CSI is used only when there is disseminated disease.
- Radiation doses are 54-59.4 Gy to Brain lesions, 45 Gy to Spine lesions, 36 Gy to CSI when indicated.
- The role of chemotherapy in adults in unclear, in pediatrics ≤4 it may be useful in delaying radiation until age > at least 3.